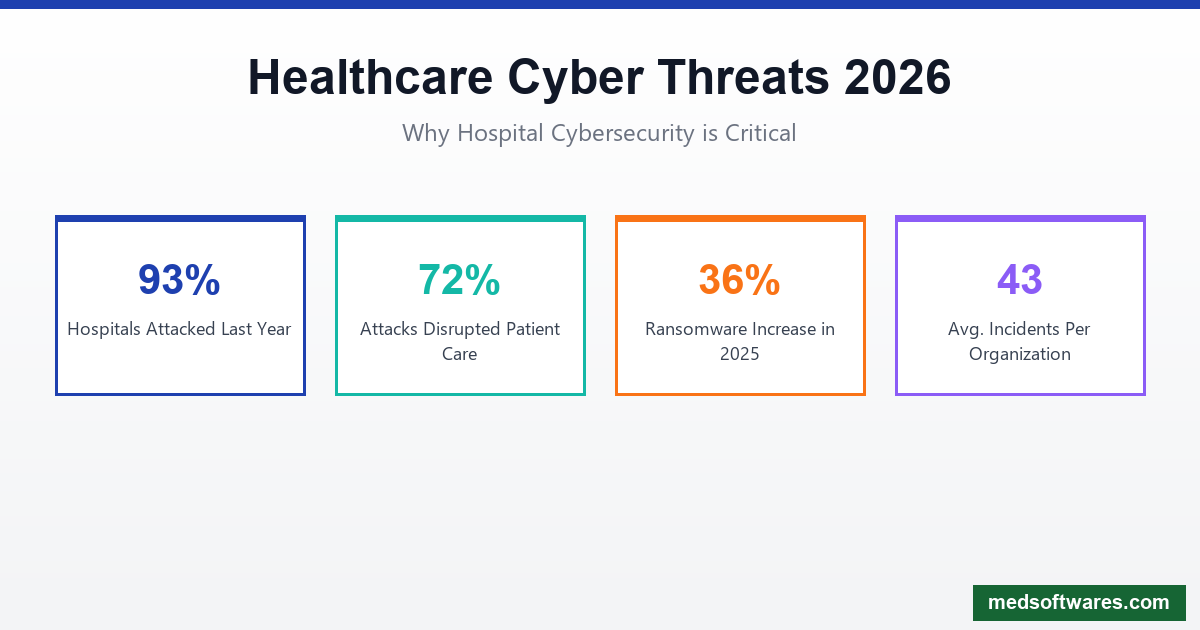
Healthcare is under siege. With 93% of U.S. healthcare organizations experiencing at least one cyberattack in the past year—averaging 43 incidents per organization—cybersecurity is no longer optional. It's a matter of patient safety and organizational survival.
The Healthcare Cybersecurity Crisis
2026 Threat Landscape
The numbers are alarming:
- 93% of healthcare organizations experienced a cyberattack last year
- 72% of incidents disrupted patient care
- 36% increase in ransomware attacks in late 2025
- 40% of US healthcare systems projected to face ransomware by 2026
- 60% of hospitals may experience care delivery disruptions
- 80% of stolen patient records come from third-party vendors
Why Healthcare is a Prime Target
High-Value Data: Medical records are worth 10-50x more than credit card data on the dark web.
Critical Operations: Hospitals can't afford downtime, making them likely to pay ransoms.
Legacy Systems: Many healthcare organizations run outdated, vulnerable software.
Complex Networks: Multiple connected devices and systems create attack surfaces.
Resource Constraints: Smaller hospitals often lack dedicated security staff.
Top Cybersecurity Threats in 2026
1. Ransomware
The Threat: Malicious software encrypts your data and demands payment for the decryption key.
Impact on Healthcare:
- EHR systems locked, patient records inaccessible
- Surgical and diagnostic equipment disabled
- Ambulances diverted to other hospitals
- Patient safety compromised
Prevention Strategies:
- Regular, tested backups (offline and offsite)
- Network segmentation
- Email filtering and phishing training
- Endpoint detection and response (EDR)
- Incident response planning
2. Phishing Attacks
The Threat: Deceptive emails trick staff into revealing credentials or installing malware.
Healthcare-Specific Risks:
- Fake vendor invoices
- Spoofed insurance communications
- Fraudulent patient inquiries
- Impersonated executives
Prevention Strategies:
- Security awareness training
- Email authentication (DMARC, DKIM, SPF)
- Multi-factor authentication
- URL and attachment scanning
- Reporting mechanisms for suspicious emails
3. Shadow AI
The Threat: Staff using unauthorized AI tools with patient data, bypassing security controls.
The Reality: 23% of clinicians use non-sanctioned AI solutions for basic tasks.
Prevention Strategies:
- Approved AI tool list
- Clear policies on data use
- Monitoring for unauthorized tools
- Secure alternatives that meet clinical needs
4. Internet of Medical Things (IoMT) Vulnerabilities
The Threat: Connected medical devices with security flaws.
Alarming Statistic: 89% of healthcare organizations have IoMT devices with known exploitable vulnerabilities linked to ransomware.
At-Risk Devices:
- Infusion pumps
- Patient monitors
- Imaging equipment
- Connected diagnostic tools
- Building management systems
Prevention Strategies:
- Device inventory and risk assessment
- Network segmentation for medical devices
- Regular firmware updates
- Manufacturer security requirements
- Monitoring for anomalous behavior
5. Third-Party Vendor Risks
The Threat: Attackers target vendors to access multiple healthcare organizations.
The Reality: Over 80% of stolen patient records come from third-party breaches.
Prevention Strategies:
- Vendor security assessments
- Business Associate Agreements (BAAs)
- Minimum necessary access principles
- Continuous monitoring of vendor connections
- Incident notification requirements
Essential Security Features for Healthcare Software
Access Controls
Role-Based Access (RBAC):
- Define permissions by job function
- Principle of least privilege
- Separate duties for critical functions
- Regular access reviews
Authentication:
- Multi-factor authentication (MFA)
- Single sign-on (SSO) with security
- Session timeouts
- Account lockout policies
- Biometric options where appropriate
Data Protection
Encryption:
- Data at rest (AES-256)
- Data in transit (TLS 1.3)
- Database encryption
- Backup encryption
- Mobile device encryption
Data Loss Prevention:
- PHI detection and classification
- Outbound content monitoring
- USB and removable media controls
- Cloud storage restrictions
- Print tracking
Audit and Monitoring
Logging Requirements:
- User access to patient records
- System configuration changes
- Failed login attempts
- Data exports and downloads
- Administrative actions
Real-Time Monitoring:
- Security Information and Event Management (SIEM)
- Intrusion detection systems
- Network traffic analysis
- Behavioral analytics
- Alert correlation
Incident Response
Essential Capabilities:
- Automated threat detection
- Isolation of affected systems
- Forensic data preservation
- Communication workflows
- Recovery procedures
HIPAA Security Rule Compliance
Administrative Safeguards
| Requirement | Implementation | |------------|----------------| | Security Officer | Designated responsible person | | Risk Assessment | Annual analysis of vulnerabilities | | Workforce Training | Regular security awareness education | | Access Management | Procedures for granting/revoking access | | Incident Procedures | Response and reporting protocols | | Contingency Planning | Backup, disaster recovery, emergency mode | | Business Associates | Contracts with security provisions |
Physical Safeguards
| Requirement | Implementation | |------------|----------------| | Facility Access | Badge systems, visitor logs | | Workstation Use | Screen locks, privacy screens | | Workstation Security | Secure locations, cable locks | | Device Controls | Hardware inventory, disposal procedures |
Technical Safeguards
| Requirement | Implementation | |------------|----------------| | Access Controls | Unique user IDs, auto-logoff | | Audit Controls | Activity logging, review procedures | | Integrity Controls | Data validation, checksums | | Transmission Security | Encryption, secure protocols |
2026 HIPAA Updates
The Office for Civil Rights proposed new HIPAA Security Rule requirements in January 2025:
- Mandatory encryption for all PHI
- Multi-factor authentication required
- 72-hour incident reporting to HHS
- Annual compliance audits
- Network segmentation requirements
- Penetration testing mandates
Building a Security Program
Zero Trust Architecture
"Never trust, always verify" applies to every user and device:
- Verify Every Access Request: No implicit trust
- Least Privilege Access: Minimum necessary permissions
- Assume Breach: Design for containment
- Continuous Validation: Ongoing authentication
Implementation Steps
Phase 1: Assessment (Month 1)
- Inventory all systems and data
- Identify vulnerabilities
- Assess current controls
- Prioritize risks
Phase 2: Foundation (Months 2-3)
- Implement MFA everywhere
- Enable encryption
- Deploy endpoint protection
- Establish logging
Phase 3: Enhancement (Months 4-6)
- Network segmentation
- SIEM deployment
- Incident response planning
- Staff training program
Phase 4: Maturity (Ongoing)
- Continuous monitoring
- Regular testing
- Policy updates
- Threat intelligence integration
Security Awareness Training
Essential Topics:
- Phishing recognition
- Password best practices
- Data handling procedures
- Social engineering awareness
- Incident reporting
- Mobile device security
Training Frequency:
- Initial onboarding training
- Annual refresher courses
- Monthly security tips
- Simulated phishing exercises
- Incident-triggered updates
Emerging Security Technologies
Quantum-Safe Encryption
Quantum computers threaten current encryption. Hospitals must prepare:
- Post-quantum algorithms: New encryption standards
- Crypto-agility: Ability to swap algorithms quickly
- Long-term data protection: Encrypt now against future threats
AI-Powered Security
Artificial intelligence enhances detection and response:
- Behavioral analytics: Detect unusual user activity
- Threat prediction: Anticipate attacks before they happen
- Automated response: Contain threats in seconds
- False positive reduction: Focus on real threats
Federated Learning
Train AI models without centralizing sensitive data:
- Local processing: Data stays at the hospital
- Shared insights: Models improve across organizations
- Privacy preservation: No PHI leaves your network
HospitalOS Security Features
HospitalOS is built with security as a foundation:
Data Protection
- AES-256 encryption for all stored data
- TLS 1.3 for data transmission
- Encrypted backups with tested recovery
- Data masking for non-production environments
Access Security
- Role-based access control with granular permissions
- Multi-factor authentication support
- Single sign-on integration
- Session management with automatic timeouts
- IP whitelisting options
Audit & Compliance
- Comprehensive audit logs for all actions
- HIPAA compliance built-in
- Tamper-evident logging
- Report generation for compliance audits
- Data retention policies enforcement
Offline Security
- Local data encryption on devices
- Secure sync when connectivity returns
- Remote wipe capability
- Offline audit logging
Why Choose HospitalOS
- Security-first design from the ground up
- No cloud dependency for sensitive data
- Regular security updates included
- Compliance documentation provided
- One-time pricing from $799
Incident Response Planning
Before an Incident
- Create Response Team: IT, legal, communications, clinical leadership
- Document Procedures: Step-by-step response playbooks
- Establish Communication: Internal and external notification templates
- Practice Regularly: Tabletop exercises and simulations
- Maintain Backups: Test restoration procedures quarterly
During an Incident
- Detect & Contain: Isolate affected systems immediately
- Preserve Evidence: Don't destroy forensic data
- Assess Impact: Determine scope and affected data
- Notify Stakeholders: Leadership, legal, potentially regulators
- Communicate Appropriately: Staff, patients, media if needed
After an Incident
- Full Recovery: Restore systems from clean backups
- Root Cause Analysis: Understand how it happened
- Improve Controls: Implement additional safeguards
- Update Plans: Incorporate lessons learned
- Regulatory Reporting: File required breach notifications
Conclusion
Healthcare cybersecurity is a patient safety issue. With attacks increasing and regulations tightening, hospitals must invest in robust security measures.
Key actions for 2026:
- Implement MFA across all systems
- Encrypt everything at rest and in transit
- Train staff continuously
- Monitor actively for threats
- Plan for incidents before they happen
HospitalOS provides enterprise-grade security designed for healthcare:
- Built-in compliance for HIPAA and local regulations
- Encryption everywhere as standard
- Offline capability reduces attack surface
- One-time pricing from $799
Protect your patients. Protect your organization.
![Healthcare Cybersecurity for Hospitals: Complete Protection Guide [2026]](/_next/image?url=%2Finfographics%2Fhealthcare-cybersecurity-stats-2026.png&w=2048&q=75)

![Medical Inventory Management Software for Hospitals: Complete Guide [2026]](/_next/image?url=%2Finfographics%2Fmedical-inventory-management-stats.png&w=2048&q=75)
